
The use of electricity in medicine has a variety of common applications and origins that go back decades. Whether it’s a cardiac pacemaker, a defibrillator or an implanted stimulator, electrotherapy provides a number of well-established benefits – one of which is pain relief and muscle rehabilitation.
The first step for those considering electrotherapy to treat pain and muscle conditions is knowing that there are three primary options available. From least invasive to most invasive, these include transcutaneous, percutaneous and implantable.
The most widely used group of electrotherapy devices fall into the transcutaneous category – also known as TENS (Transcutaneous Electronic Nerve Stimulation). But with options ranging from prescription-only units offering high-frequency signals of 5000 Hz to over-the-counter units offering low-frequency signals of 50 Hz, it can be challenging to know when to pick one over another. A review of the various signal types, however, provides a way to begin discerning the optimal applications for different devices.
Before diving into this analysis, it’s important to clear up a common misperception – that all TENS devices are the same. This is like saying one pill is just like any other. Categorically, these devices are used to treat chronic and acute pain, and, in some cases, muscle conditions.
The one attribute all transcutaneous devices do have in common is that they transmit electrical signals through the skin by way of electrode pads that adhere on top of the treatment area. The challenge – the confusion, really – is that the category itself and a specific device type within the category both get referred to as TENS.
It’s a bit like facial tissue being called Kleenex®. There is a specific brand named Kleenex within the facial tissue category, but many people have gotten used to calling all facial tissues “Kleenex.” In this article, any mention of TENS will be referring to the TENS category unless stated otherwise.
Each type of signal offered by TENS units has a place in the arsenal of tools available to healthcare providers who have patients with painful musculoskeletal conditions. The “right” signal will depend largely on the diagnosis and prior treatment outcomes.
Knowing that signals are “tuned” for different purposes – for instance, causing a muscle to contract or preventing a nerve from transmitting pain signals – presents a guide to understanding the therapeutic value of each. This is also the first step to determining the best device for the patient.
1. Neuromuscular Electronic Stimulation (NMES)
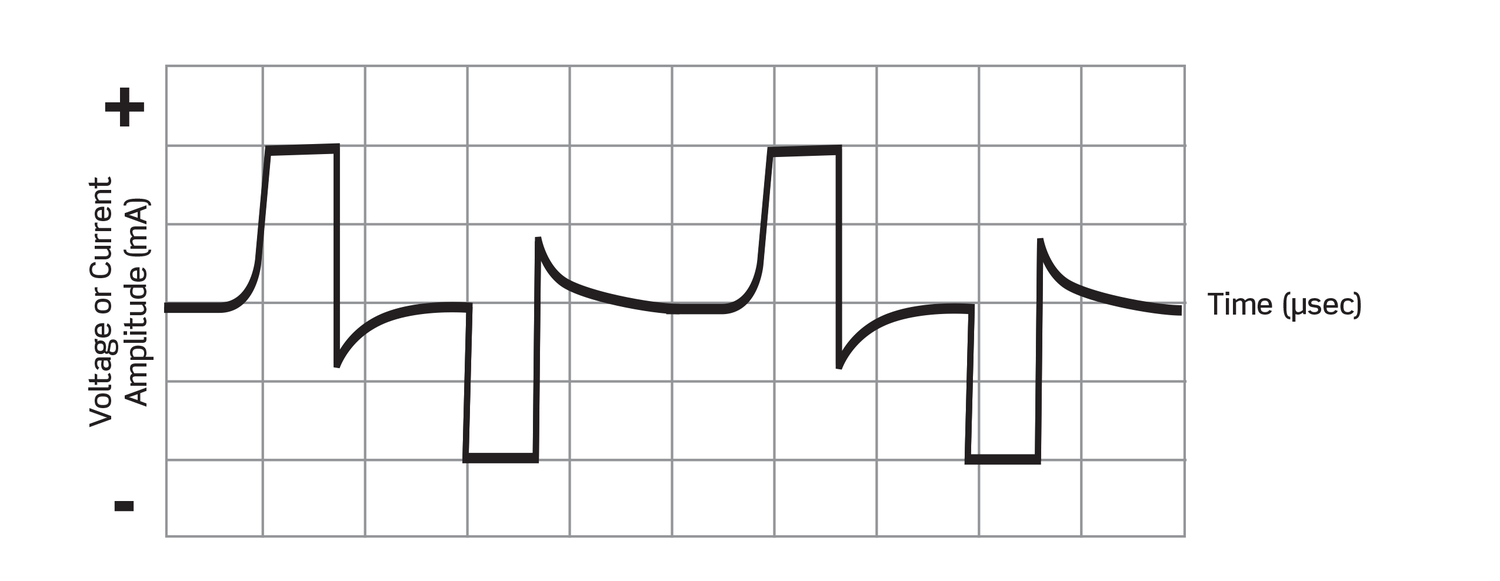
NMES uses alternating low-frequency signals (<100 Hz) to treat muscle tissue. These low-frequency signals cause skeletal muscle to contract and release in a pattern that acts as a blood and lymphatic fluid pump – i.e., the blood pump mechanism of action. The key benefits of this contract-and-release pattern are that it prevents disuse atrophy, increases circulation and re-educates tissue.
Treatments are usually short and taken daily at home or in-clinic. Intensity settings are adjusted by the user. Treatment with two electrodes may be sufficient, or patients can use four electrodes to treat a larger area.
Waveform
Indications for NMES
Contraindications (see below)
2. TENS Stimulation (the Device Type, not the Category)
A standard TENS unit typically delivers a low-frequency (<50 Hz) alternating current to a focused treatment area. Due to the nature of low-frequency, however, these signals have a low capacity to overcome skin resistance – resulting in these units only providing pain relief via the Gate Control Theory while being worn. As such, these units are often worn continuously. Intensities are user-adjustable on most devices.
Waveform
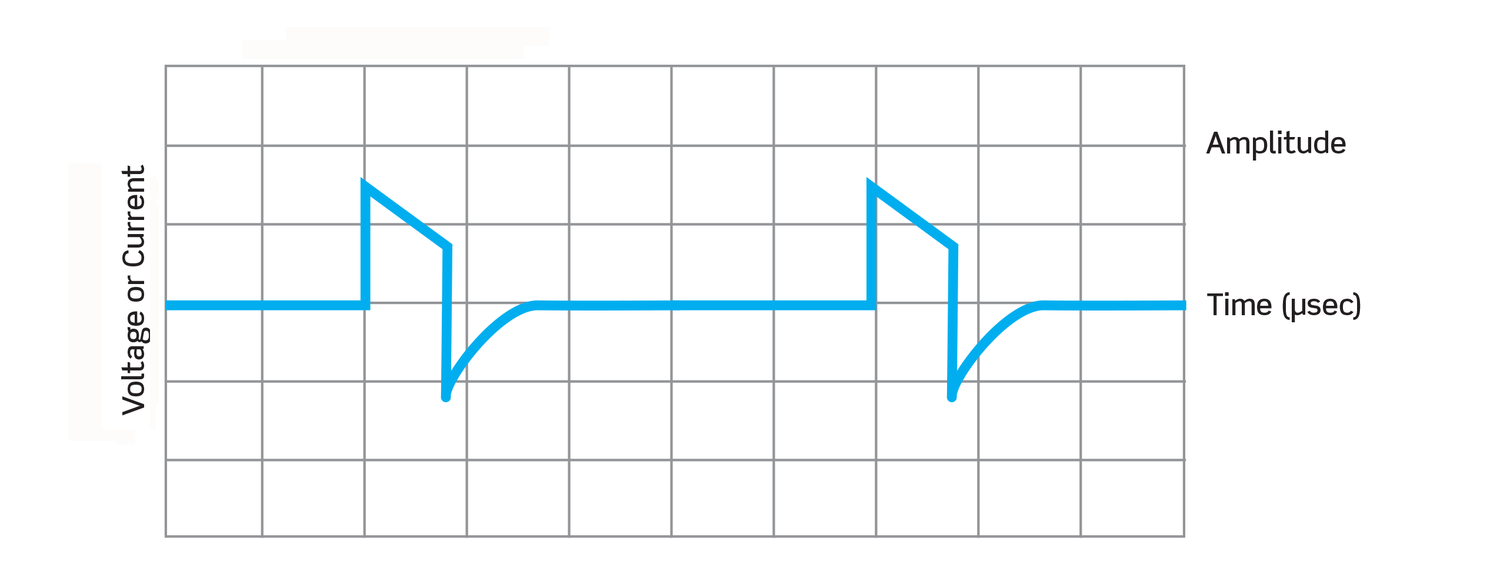
Indications for TENS
Contraindications (see below)
3. Interferential Stimulation (INF)
Interferential therapy uses two slightly different high-frequency signals (>5000 Hz) that intersect within the body to create an area of interference – a “sweet spot” in the treatment area where the therapeutic benefit is most pronounced.
The nature of high-frequency assures that these signals are able to overcome the skin’s natural resistance and reach nerves deep in the tissue, providing fast-acting pain relief via the Gate Control Theory. As an added advantage, they also offer long-lasting pain relief via the release of endogenous opiates.
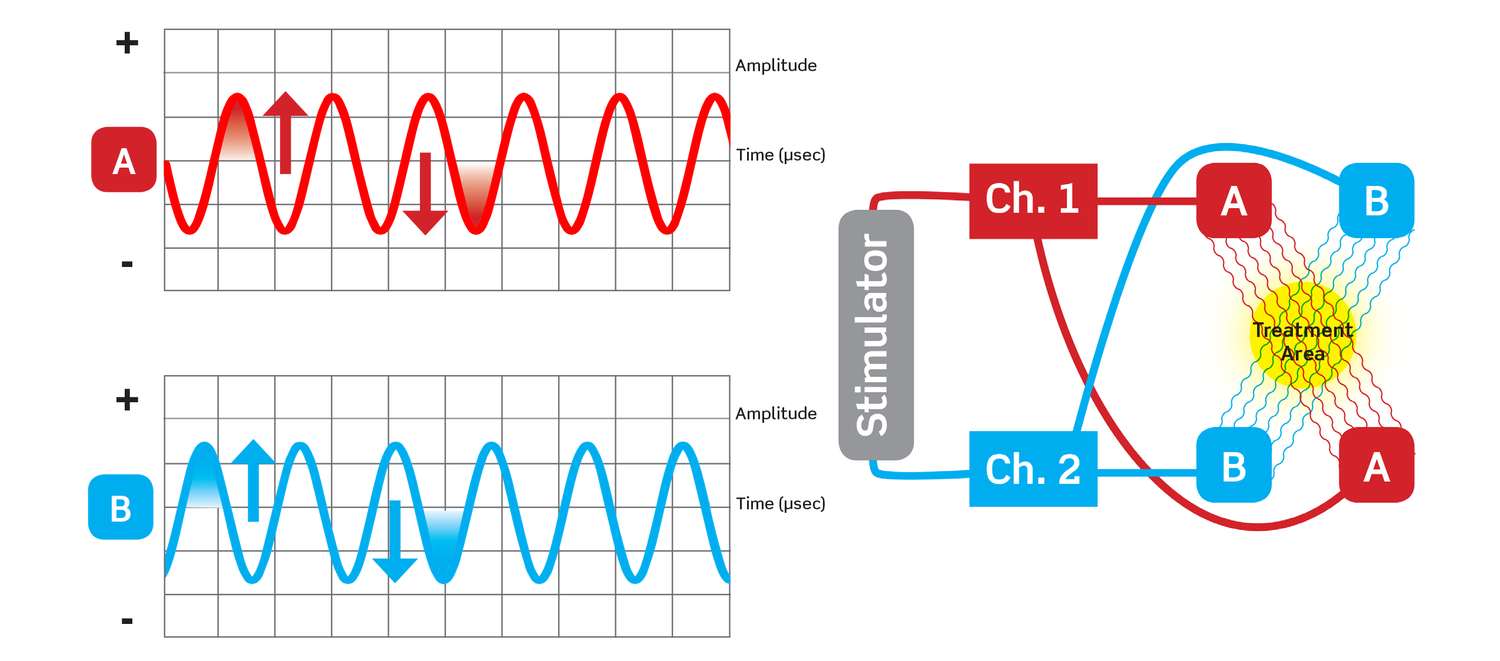
INF treatments are generally short, about 30 minutes, and taken daily at home or in a physical therapy clinic. Signal intensities are adjustable by the user or clinician.
Indications for INF
Contraindications (see below)
4. Premodulated Interferential Stimulation (Premodulated INF)
Premodulated INF differs from traditional INF in that the current for each channel is pre-mixed within the device, as opposed to inside the body. The key benefit of this type of stimulation is that it creates an expanded treatment area.
Because signals are pre-mixed, the area of interference stretches between each set of electrodes, not just where signals intersect. The result is that premodulated INF provides a significantly broader area of pain relief, allowing for the treatment of large body areas particularly when using four electrodes.
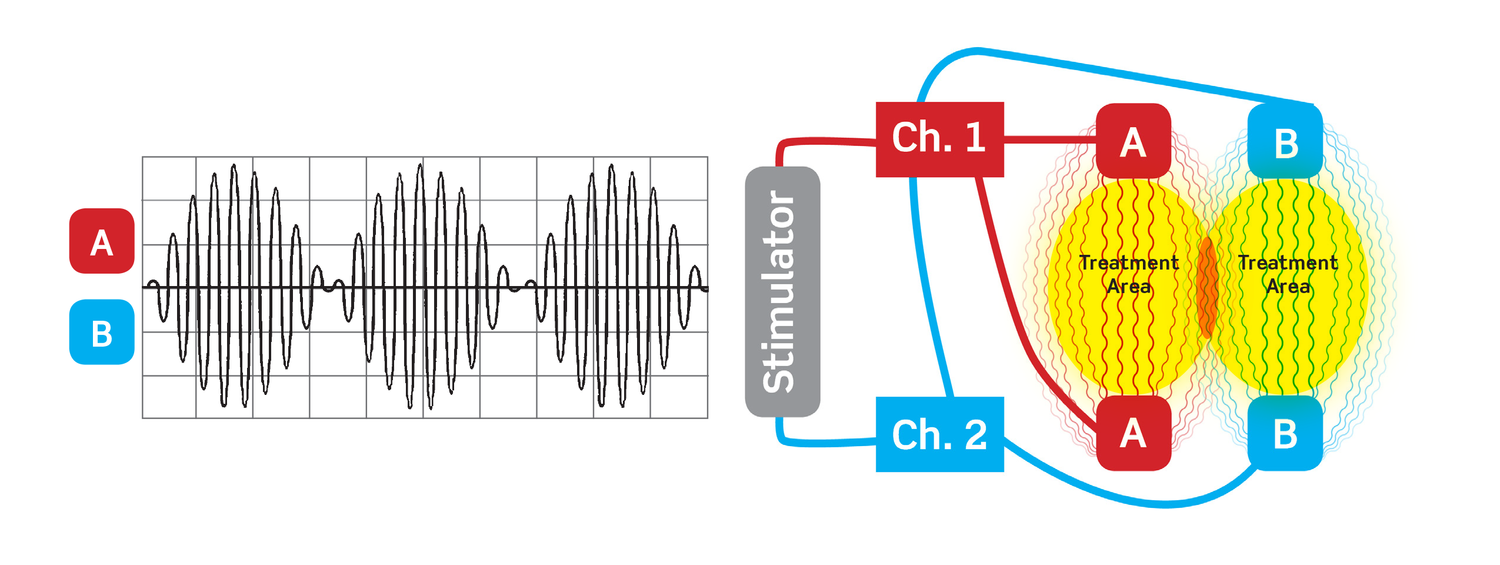
While the primary value is for larger areas, it can also be useful when treating small muscle groups or joints (elbow, ankle, foot) where only two electrodes can be used due to space limitations. For devices that are able to offer more than one signal type, an additional advantage of premodulated INF is that the electrode pads do not need to be repositioned for muscle therapy (via NMES).
Premodulated INF treatments are generally short, about 30 minutes, and taken daily at home or in a physical therapy clinic. Signal intensities are adjustable by the user or clinician.
Indications for Premodulated INF
Contraindications (see below)
5. Galvanic Stimulation
Galvanic stimulation applies high-voltage direct current to reduce edema in acute injuries associated with major tissue trauma. Direct current creates an electrical field over the treated area that, theoretically, changes blood flow. The positive pad behaves like ice, causing reduced circulation to the area and a reduction in swelling. The negative pad behaves like heat, causing increased circulation and faster healing.
Galvanic treatments are generally taken daily at home, although patients may periodically take them in-clinic.
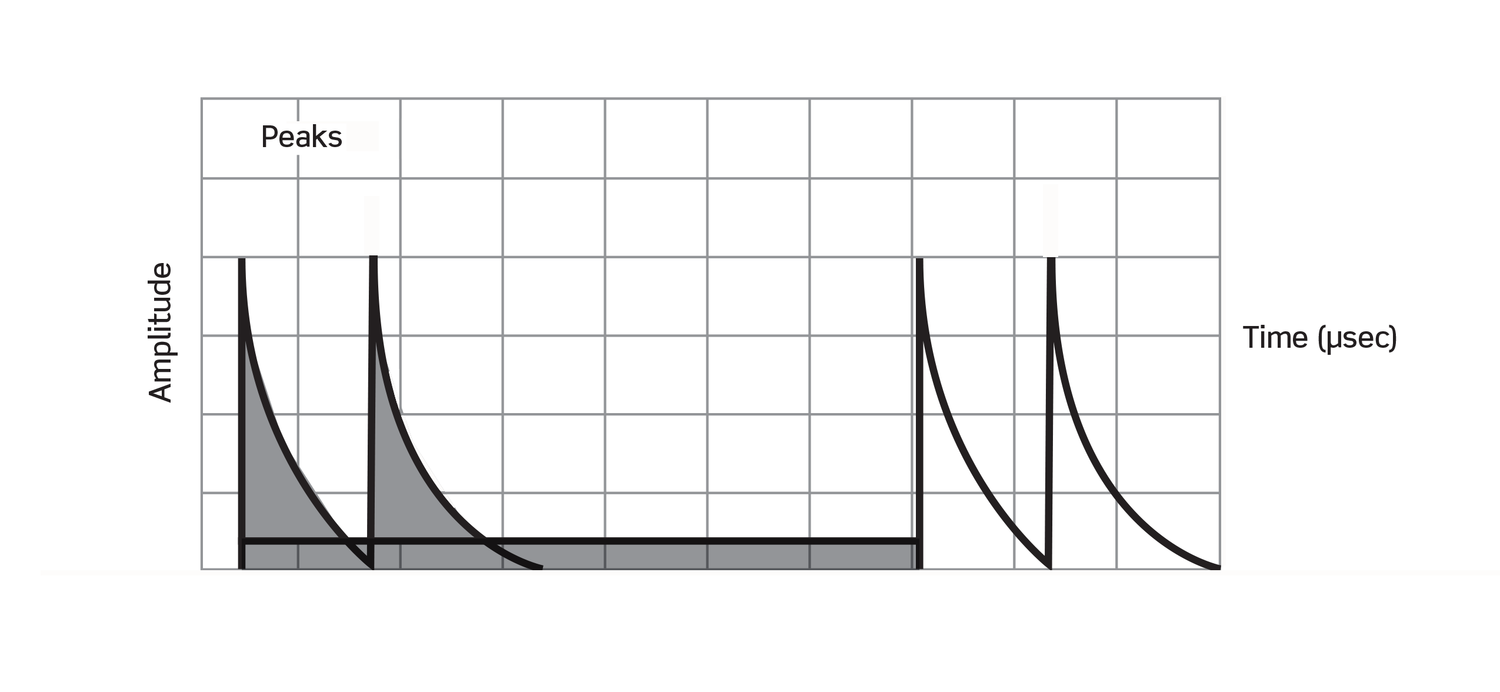
Waveform
Indications for Galvanic
Electrotherapy devices, regardless of device type, share the following contraindications:
Knowing that all transcutaneous electrotherapy devices are not the same is the first step in understanding the TENS category. Taking a deeper dive into what makes them different reveals that there are five signal types with varying indications for use – the distinctions of which can help healthcare providers hone in on a particular therapy, and ultimately device, that will be most beneficial for each patient’s condition.
Those wishing to read more about TENS therapy may want to review the scientific articles listed below or visit PubMed for additional articles on electrotherapy:
Do you have experience with TENS electrotherapy devices? If so, feel free to add your questions or comments.